

That total duration was then divided in half, and half of the time was allocated to the prior INR group and the other half of the time was allocated to the new INR group. The time that each patient stayed in each INR group was calculated by taking the duration between when a patient was in one INR group to when that same patient had an INR score that was in another INR group. Assignment of an event to an INR group was made using the first INR during the event or the most recent INR level within 7 days prior to the occurrence of the thromboembolic or bleeding event. The INR-specific incidence density was calculated as the ratio of the number of thromboembolic or bleeding events that occurred in each INR group to the total amount of time (patient-years) that each patient stayed in each INR group, according to the method described by Frits R Rosendaal, et al., 1993. INR level was classified into the following 6 groups for analysis: 4.5. We collected demographic data, clinical data, types of mechanical valve, INR levels, and warfarin dose. We then proposed the total sample size of 200 patients. By using the proportion of outcome at 0.062, variance of 0.005, with the power of 90% (a type II error of 0.10), a type I error of 0.05, The sample size of all groups was 192 patients. The average proportion of thromboembolism and bleeding outcome from the calculation was 0.062 and variance of proportion was 0.005.

The calculated ratio of n for the 6 INR groups were 1: 6: 4.2: 4: 4: and 0.8. From the estimation of proportion of patients in each INR group, we calculates the ratio of ni/n 1 assuming that n 1 which is the number of patients in the group with the lowest INR (INR < 2) = 1. We calculated sample size by G group Chi-square test comparing proportions in C Categories formula by nQuery program (Statistical Solutions Ltd., Cork, Ireland).
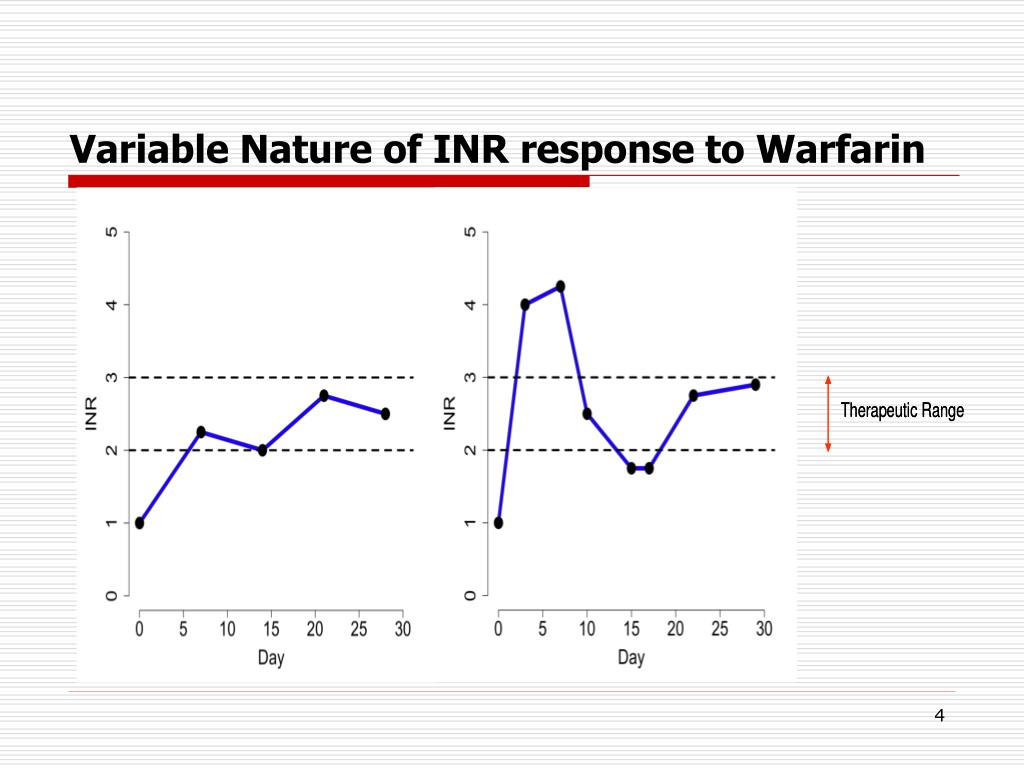
They reported the incidence of thromboembolic and bleeding events in the 4.5 INR groups to be 0.319, 0.067, 0.02, 0.025, 0.033, and 0.247, respectively. We calculated sample size based on the results of a previous publication by Marieke Torn, et al., 2009. We studied patients who underwent mechanical mitral valve replacement and received warfarin therapy at Siriraj Hospital during the 2011 to 2015. Study population and sample size calculation Accordingly, the aim of this study was to identify the optimal INR level for warfarin therapy after mechanical mitral valve replacement in Thai patients. However, the currently available data from Thai population are insufficient for defining the optimal INR level for anticoagulant therapy in Thai mechanical valve recipients. The few studies that were conducted in Asian populations who received mechanical heart valve replacement generally recommended a lower INR level as being appropriate for anticoagulant therapy. There is no clear explanation for the increased risk of intracerebral bleeding in Asian population. Asian population had a greater proportion of intracerebral bleeding as a stroke subtype when compared to Caucasians. Previous data have shown that Asian population with atrial fibrillation who received warfarin has an increased risk of intracranial hemorrhage up to 4 times compared to Caucasians. These data were based on results from studies conducted in Western countries however and according to our review of the literature, data regarding the safety of warfarin in Asian populations remain insufficient. A target INR range of 2.5–3.5 is the current recommendation in patients who have undergone mechanical mitral valve replacement. Current American and European clinical guidelines recommend a higher international normalized ratio (INR) for anticoagulant therapy after mechanical mitral valve replacement, because higher rates of thromboembolic complications were reported when the mechanical valve was in the mitral position, as compared to when the mechanical valve was in the aortic position. Risk of thromboembolism and bleeding is commensurate with the level of anticoagulation. However, bleeding complications that result from excess dose of anticoagulants adversely impacts patients’ quality of life and can cause unnecessary morbidity and mortality. Lifelong oral anticoagulation therapy for prevention of thromboembolic events is recommended in all patients who undergo mechanical heart valve replacement.


 0 kommentar(er)
0 kommentar(er)
